
Bacteria overgrowth can be secondary to proton-pump inhibitors and histamine type 2 receptor antagonists for stress ulcer prophylaxis, which neutralized gastric pH and promotes colonization of the upper gastrointestinal tract. This biofilm can be dislodged and delivered to the lower respiratory tract through mechanical suctioning or high-pressure airflow, leading to pneumonia in a susceptible host. Artificial airway inhibits gag reflex and ciliary functions and provides a substrate for growth of biofilm which acts as a reservoir for pathogens. Mechanical defenses, such as ciliary motion and mucus secretion, can be altered in an intubated patient. This depends on the number, type, and virulence of the bacteria as well as natural host defenses such as mechanical factors and humoral and cellular immunity. There are few mechanisms suggested for development of ventilator-associated pneumonia: (1) most commonly it is thought to be a progression from colonization of the upper airway, leading to tracheal colonization, then tracheitis, and finally pneumonia. However, this distinction is not helpful in children who are frequently admitted to the hospital.

In addition, early pneumonia (less than 4 days after admission to the hospital) is most likely from antibiotic-sensitive community-acquired organisms, and late pneumonia (more than 4 days) is more likely due to antibiotic-resistant organisms. Nosocomial viruses and fungi are rare causes of pneumonia in immunocompetent hosts. Anaerobic bacteria are an uncommon cause of Ventilator-associated pneumonia but can play a role in polymicrobial infections, particularly when pneumonia is due to aspiration. Other pathogens include the Streptococcus, Enterobacteriaceae, and Acinetobacter species. Patients in a NICU have a risk of Enterococcus species and group B Streptococcus as well. aeruginosa, and Klebsiella and Enterobacter species. Īrtificial airways become colonized with pathogenic bacteria soon after intubation or tracheostomy, and the major pathogens include both gram-positive and gram-negative bacteria: S. The most common organisms were Staphylococcus aureus (28.4 %), Pseudomonas aeruginosa (25.2 %), and other gram negatives (26.6%). In a large retrospective review done in the ICU settings of three hospitals, the microbiology was the same across adult and pediatric hospitals. However polymicrobial infections are increasing. Ventilator-associated pneumonia is typically bacterial and from a single organism. For convenience, the infection of an artificial airway after colonization is either diagnosed as tracheitis or ventilator-associated pneumonia. Ventilator-associated pneumonia is part of a spectrum of upper airway infection after the of an artificial airway with bacteria. Tracheitis Versus Ventilator-associated Pneumonia Infants and children are usually classified to the first category.
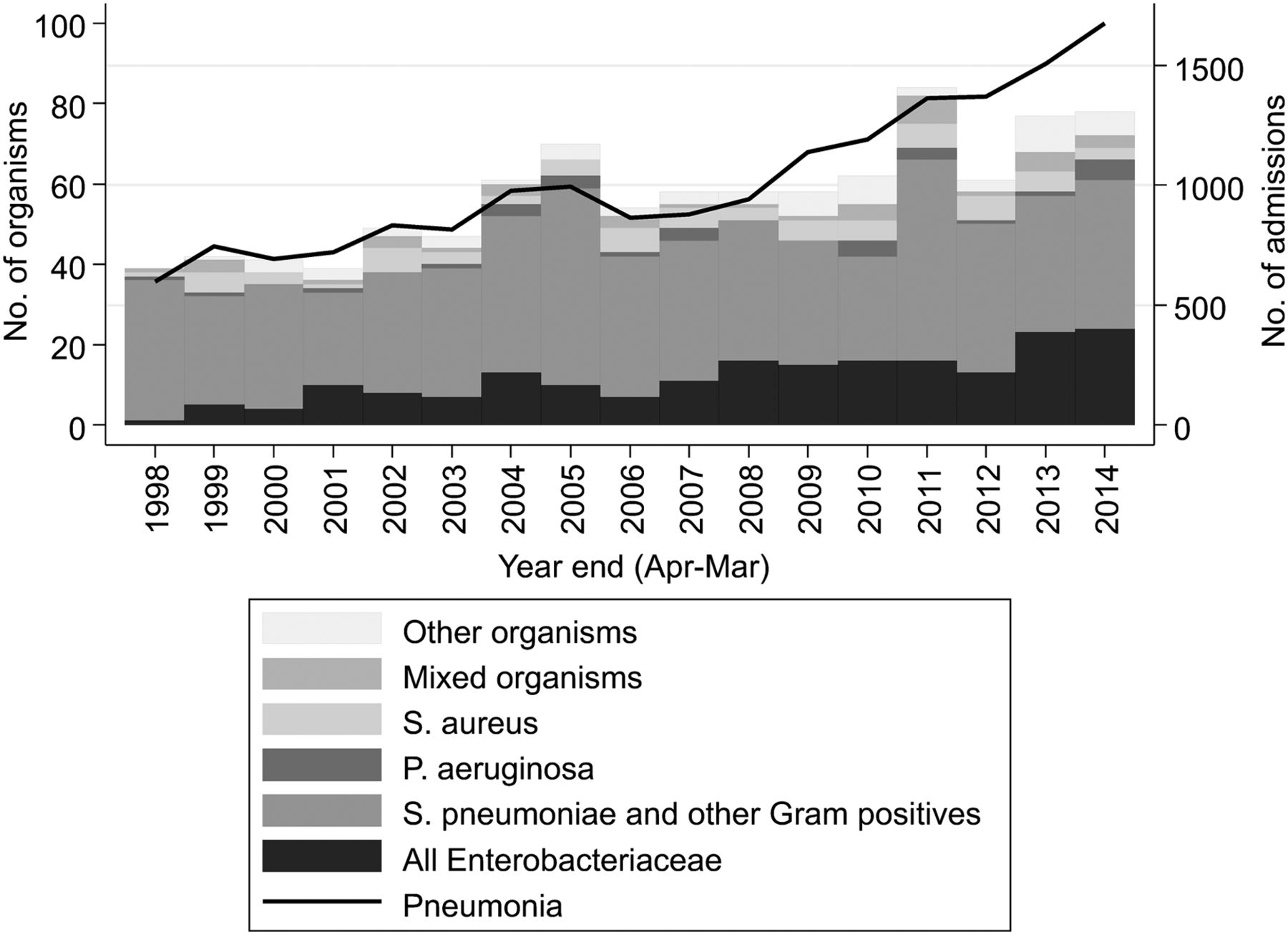
They have classified it as three types: (1) clinically defined, (2) pneumonia with laboratory findings, and (3) pneumonia in immunocompromised patients. In 2008, the Centers for Disease Control (CDC) and National Healthcare Safety Network (NHSN) have attempted to provide reproducible criteria for the surveillance of ventilator-associated pneumonia. It is difficult to diagnose ventilator-associated pneumonia in any patient, and this holds true in young children, particularly in the neonatal ICU population. Ĭhildren with artificial airways, such as a tracheostomy tube for management of chronic respiratory failure or an endotracheal for acute airway management, are at risk for ventilator-associated pneumonia. There is limited data on infants and children with VAP, so most of the information is extrapolated from adult studies. In neonates, the rate of ventilator-associated pneumonia is inversely proportional to birth weight. Generally, the rate of pneumonia in pediatric intensive care units (PICU) is lower than in adult intensive care units (ICU). It accounts for 7% to 32% of healthcare-associated infections and 10% of all pediatric device-related infections reported to the National Healthcare Safety Network (NHSN). Ventilator-associated pneumonia (VAP) is a term used to describe pneumonia (lung infection) that develops in a patient who has been on mechanical ventilation for more than 48 hours. Ventilator-associated pneumonia is the second most common hospital-acquired infection among pediatrics and neonatal intensive care unit patients.


 0 kommentar(er)
0 kommentar(er)
